If you are wondering, “does TRICARE cover mental health services?” the answer is yes! TRICARE offers mental health and substance use disorder (SUD) services for you and your family. These services are available during times of stress, depression, grief, anxiety, mental health crises, and issues related to alcohol or drug misuse or abuse. This is great news if you or a loved one need support. TRICARE is a health care program for service members, retirees, and their families. It provides many benefits, including comprehensive mental health care.
What Mental Health Services Does TRICARE Cover?
TRICARE covers a wide range of mental health services. Here are some of the key services they offer:
- Counseling and Therapy: Firstly, you can talk to a counselor or therapist to help with feelings, stress, and problems. This can include individual therapy, group therapy, and family therapy.
- Medications: Secondly, if you need medicine to help manage your mental health, TRICARE can help pay for it. This includes medications for depression, anxiety, and other conditions.
- Hospital Stays: Thirdly, if you need to stay in the hospital to get better, TRICARE covers the cost. This is important if you need more intensive treatment.
- Specialized Treatments: Lastly, TRICARE also covers other types of treatments, like TMS Therapy, inpatient programs, outpatient programs, and residential treatment centers.
Who Is Covered by TRICARE?
TRICARE covers many people, including:
- Active-Duty Service Members: If you are currently serving in the military, you are covered by TRICARE.
- Retired Service Members: If you have retired from the military, you and your family can still get TRICARE coverage.
- Family Members: Spouses and children of service members are also covered. This means your whole family can get the mental health services they need.
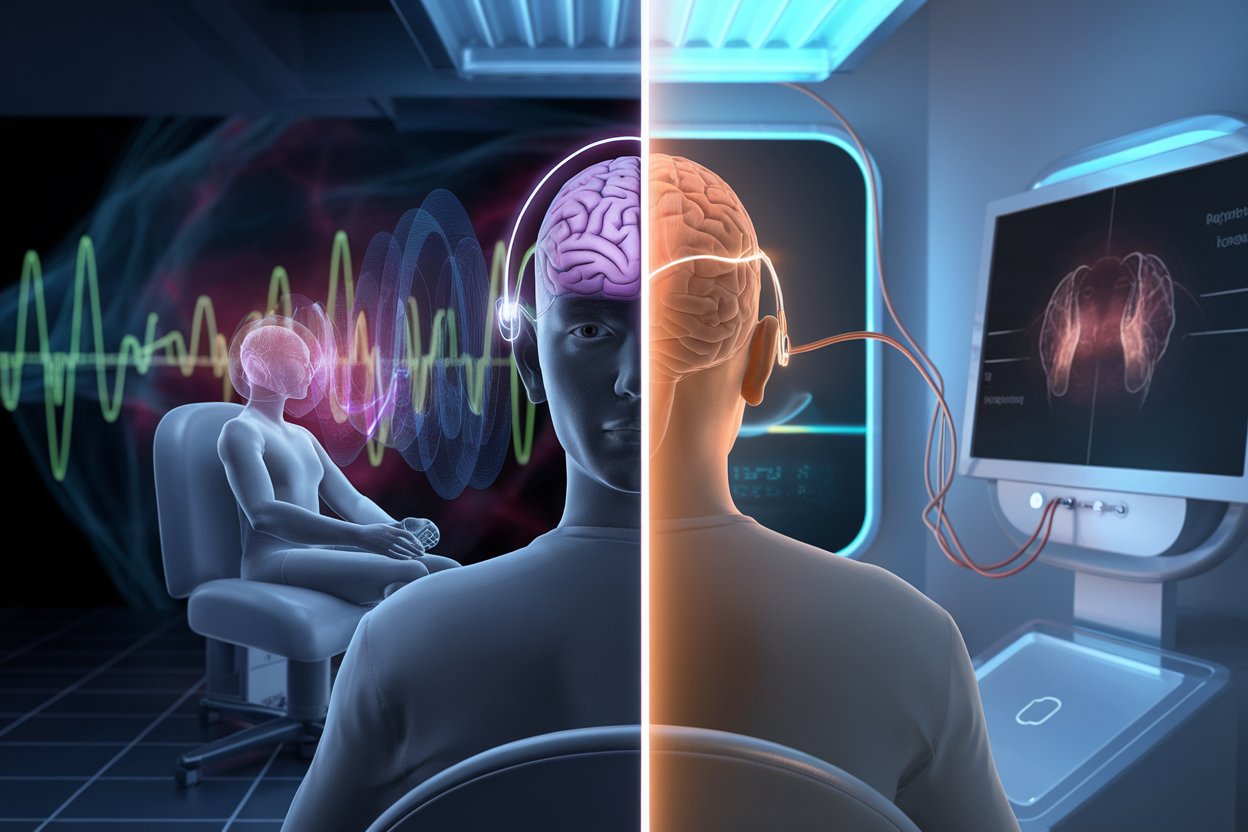
What Is TMS Therapy?
TMS stands for Transcranial Magnetic Stimulation. It is a treatment that helps people with depression when other treatments haven’t worked. TMS uses magnets to stimulate parts of the brain that are involved in mood regulation. This can help improve symptoms of depression and other mental health issues.
Is TMS Therapy Covered by TRICARE?
Yes, TRICARE may cover TMS therapy under certain conditions. Whether TRICARE covers TMS therapy depends on your specific plan and medical needs. Some TRICARE plans may cover TMS if it is medically necessary. However, it’s important to check with your TRICARE provider or contact us to see if TMS therapy is covered for you.
Why Choose American TMS Clinics?
At American TMS Clinics, we specialize in Transcranial Magnetic Stimulation (TMS) and we are an accredited TRICARE TMS Therapy provider in Phoenix, Arizona. Moreover, our team is dedicated to helping you improve your mental health. We understand that dealing with mental health issues can be challenging, and we are here to support you every step of the way.
FAQ: Does TRICARE Cover Mental Health Treatment?
1. How many mental health sessions does TRICARE cover?
TRICARE covers an unlimited number of outpatient mental health sessions as long as they are deemed medically necessary. This means you can continue receiving the help you need without worrying about hitting a session limit. Whether you need weekly therapy or more frequent visits during a crisis, TRICARE provides the necessary support for your mental health needs.
2. Does TRICARE require a referral for a psychiatrist?
Yes, TRICARE typically requires a referral from your primary care manager (PCM) to see a psychiatrist, especially for non-emergency care. This ensures that your care is coordinated and that all treatments are deemed necessary. For emergency situations, you can access mental health services immediately without a referral, but follow-up care might still require one.
3. What is not covered by TRICARE?
TRICARE does not cover services and supplies that are not medically necessary. This includes experimental procedures, unproven treatments, and certain elective services like cosmetic surgery. Additionally, TRICARE might not cover some alternative therapies unless they are part of a comprehensive treatment plan approved by your PCM.
4. Does the military pay for therapy?
Yes, through TRICARE, the military pays for therapy services for eligible members and their families. This includes individual therapy for personal mental health issues, group therapy for shared experiences, and family therapy to address family dynamics and issues. TRICARE ensures that military families have access to comprehensive mental health care to support their well-being.
5. Does TRICARE pay for TMS therapy?
Yes, TRICARE may cover TMS therapy under certain conditions. TMS, or Transcranial Magnetic Stimulation, is a non-invasive treatment for depression when other treatments have not been effective. To be covered, TMS therapy must be deemed medically necessary by your TRICARE provider. Still, it’s important to check with your TRICARE provider to see if you are eligible for this coverage and to understand the specific requirements and approval process.
Contact American TMS Clinics Today
Finally, If you are interested in finding out more about TMS therapy and if TRICARE covers it, contact American TMS Clinics today. See if you qualify for a free EEG and psychiatric evaluation. Your mental health is important, and we are here to help!
Call American TMS Clinics at (602) 922-0960 today to learn more and see if TMS therapy is right for you!